Types and Subtypes of Progressive Familial Intrahepatic Cholestasis (PFIC)
| PFIC 1 | PFIC 2 | PFIC 3 | PFIC 4 | PFIC 5 | PFIC (no #) | PFIC (no #) | |
|---|---|---|---|---|---|---|---|
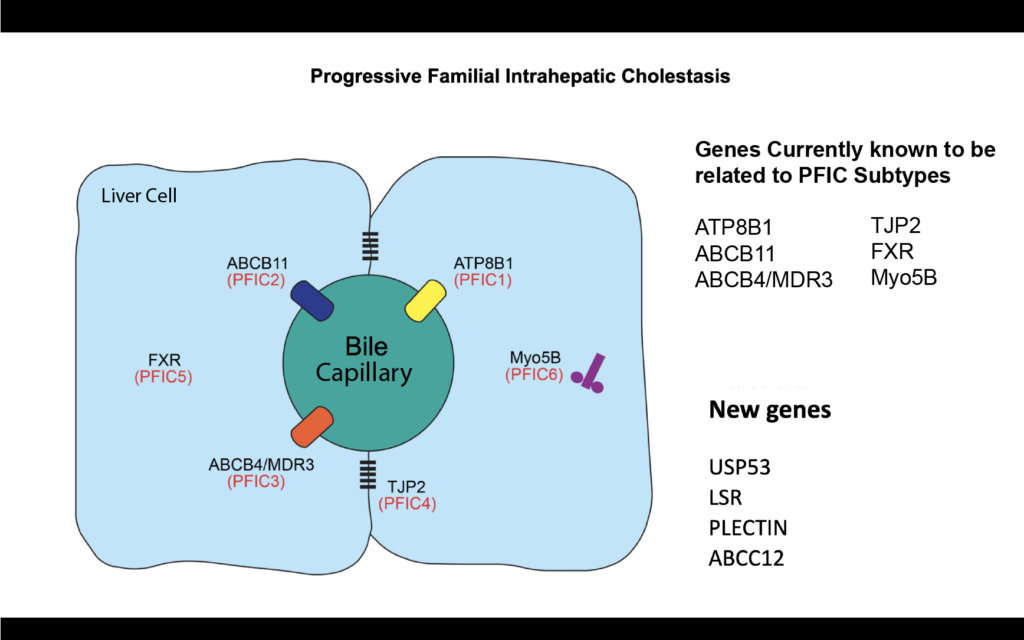
| Protein Deficiency | FIC 1 | BSEP | MDR3 | TJP2 | FXR | MYO5B | USP53 |
| Mutated Gene | ATP8B1 | ABCB11 | ABCB4 | TJP2 | NR1H4 | MYO5B | USP53 |
Note: You may see PFIC listed by number (1, 2, 3, etc.) or by it’s specific defective gene. It’s important to understand that before any of these genes were identified, PFIC was all lumped together as low ggt and high ggt PFIC. As specific genetic etiologies were identified they started to become numbers. PFIC 1 2 and 3 were the first 3 identified and those terms stuck. As research progresses and we identify many more genetic causes of PFIC, the numbering system may do away.
PFIC Types Summary
The types of PFIC involve mutations in different genes. Those mutations can be more or less severe which leads to variability in the disease even amongst the same gene. A gene is a piece of code that provides the recipe to make a specific protein. Proteins have important functions in the body, and mutations often result in deficiency or other malfunction of the coded proteins. The different types of PFIC involve mutations of different genes, and therefore different proteins. The proteins have in common that they all have functions related to bile transport from the liver to the small intestine and back. Deficiencies of these proteins cause bile build-up in the liver (“cholestasis”). For more information on the function of genes and proteins in relation to PFIC, please visit our genetics page.
More Common PFIC Types
Previously, this type was known as Byler’s disease. PFIC 1 is characterized by mutations in the ATP8B1 gene. These mutations cause a deficiency of the FIC1 protein. Deficiency of the FIC1 protein can lead to Benign Recurrent Intrahepatic Cholestasis (BRIC1) as well as PFIC1. These are now considered different levels of severity of the same condition.
It is not clear yet why exactly deficiency of the FIC1 protein causes build-up of bile in liver cells, and other symptoms of BRIC1 or PFIC1.
Characteristics and Symptoms of FIC 1 (PFIC Type 1)
- Jaundice in the first months of life
- Severe itch (pruritus) beginning in the first year of life
- High levels of serum bile acids, low GGT levels
- Fat-soluble vitamin deficiencies are common (may require testing to identify)
- Progresses to chronic liver disease and possible cirrhosis at varying rates
- Potential problems that are independent of the liver including hearing problems, irritation of the pancreas, chronic diarrhea, growth issues and chronic cough
Characteristics and Symptoms of BRIC1
- Recurrent episodes of symptoms which may be quite mild
- First sign is often pruritus, but jaundice may also occur
- The time of a first episode varies widely (records show 2 months to 47 years)
- Factors such as infection or medication may precipitate the first episode
- Frequency, duration, and severity of episodes can vary greatly
- Episodes often reduce with age
- In some cases BRIC evolves to be like PFIC1 (i.e. there are no periods of remission of the symptoms) and can progress to chronic liver disease
Mutations in the ABCB11 gene are responsible for the deficiency of the Bile Salt Export Pump (BSEP) protein. This protein works like a pump and moves bile salts out of liver cells. The deficiency of this protein directly leads to build-up of bile in liver cells, which in turn causes liver damage. Depending on the severity of the mutation, the BSEP protein is reduced or completely absent.
Characteristics and Symptoms of BSEP deficiency (PFIC Type 2)
- GGT levels are normal (see more information on GGT tests here)
- Pruritus (itch) becomes severe in the first years of life
- Cirrhosis (liver scarring) often occurs before the age of 10 years
- Milder intermittent forms (sometimes called BRIC 2) have also been identified
- There is a high risk of liver cancer in some individuals this type of PFIC which makes regular monitoring by blood test and ultrasound particularly important
Deficiency in either the FIC1 protein or the BSEP protein can lead to a milder form of PFIC called BRIC. BRIC stands for Benign Recurrent Intrahepatic Cholestasis, and depending on the protein involved can take on those symptoms of its PFIC form.
Characteristics and Symptoms of BRIC1 and 2
-
- Recurrent episodes of symptoms which may be quite mild
- First sign is often pruritus, but jaundice may also occur
- The time of a first episode varies widely (records show 2 months to 47 years)
- Factors such as infection or medication may precipitate the first episode
- Frequency, duration, and severity of episodes can vary greatly
- Episodes often reduce with age
- In some cases BRIC evolves to be like PFIC 1 or 2 (i.e. there are no periods of remission of the symptoms) and can progress to chronic liver disease
Mutations in the ABCB4 gene cause deficiency of the MDR3 protein. This protein seems to be involved in the transport of phospholipids (a type of fat) from liver cells into bile, where they bind to bile acids. Deficiency of this protein causes a lack of fats for bile acid to bind, which in turn causes injury to the tubes that drain bile from the liver. This can then lead to liver injury.
Characteristics and Symptoms of MDR3 deficiency (PFIC Type 3)
- High levels of GGT in the blood — this is an important difference from FIC1 and BSEP deficiencies
- Pruritus tends to be milder
- Bile duct damage may occur
- Gallstones and stones within the liver are common
-
There is a very wide range of severity
- PFIC 3 can occur during infancy, childhood and even into young adulthood – when it presents in childhood and young adulthood it may be with cirrhosis, an enlarged spleen or low platelets
- During pregnancy, women who are carriers for this disease can develop jaundice and itching
The following three types have been found more recently:
The TJP2 protein (Tight Junction Protein 2, sometimes called ZO2) plays a role in “tight junctions”. Tight junctions are areas where the membranes of two adjacent cells join to form a barrier. The barrier controls what molecules are able to pass between cells. Such junctions are important throughout the body, and TJP2 is not specific to the liver. A mild form of liver disease associated with mutations in the TPJ 2 gene was previously called familial hypercholanemia (which means high bile salts in blood). Only a small number of patients with PFIC caused by TJP2 mutation have been studied so far. It is not yet understood what manifestations, other than liver disease and its consequences, TJP2 deficiency patients may have.
This type of PFIC is caused by a mutation in the NR1H4 gene, which encodes the FXR (the Farnesoid X Receptor) protein. This protein is important in regulation of bile acid metabolism in the liver and intestine, as well as in other aspects of metabolism. Patients with PFIC due to FXR deficiency seem to develop rapidly progressing liver disease potentially very early in infancy. Only 4 patients have been reported so far, although it is expected more will likely be identified as this cause of PFIC is fairly newly described.
MYO5B is involved in maintaining proper functioning of cell membranes and helping to move proteins, such as BSEP, to where they are needed. MY05B has been related to intestinal disorder, cholestasis, or both. Some patients with cholestasis due to MYO5B deficiency have progressive liver disease, while others have it only intermittently.
Unidentified forms of PFIC
The mechanisms of bile formation are extremely complex. As a result, researchers anticipate they will identify more genetic causes of PFIC in the future. The identification of these possible new mutations requires state of the art genetic investigations.
Although many PFIC patients have mutations in one of the genes mentioned above, there are still PFIC patients in whom mutations are not found in any of these genes. Genetic studies are underway to try to identify genetic factors contributing to PFIC in such patients.
Learn More: Educational Webinars
We offer several educational webinars that cover PFIC genetics in detail, especially in regards to how genetics and PFIC types and subtypes are related. Check out Genetics of PFIC and Its Subtypes (2020), Genetics of PFIC by Subtype (2021) and more!
