Genetics of PFIC by Subtype
Genetics of PFIC by Subtype (2021)
SPEAKERS
Dr. Richard Thompson, Emily Ventura
Emily Ventura 00:06
Hi, welcome. I’m just gonna give a few minutes for attendees to enter the room. I guess I’ll take the early moment to say thank you very much to Dr. Thompson and Dr. Bull for taking the time to speak to us today. It’s one of the most anticipated topics, probably one of the more complex ones, of a very complex panel, to address. So we appreciate you taking the time. So we’ll go ahead and get started. Real quickly the slides. If you’re using our translation software, remember, in the top left hand corner of your screen, there’s the Live button. You click that it’ll open up a new tab, which will be the Wordly translation
. You can pick your language from the drop down menu, and you’ll have a closed captioning service. Remember that it is software based, AI based, so it may not be perfect, but hopefully it’s helpful. These sessions are for information educational purposes only. So if you have any questions related to your own health or the health of your child, please consult your doctors. Zoom is not a HIPAA compliant platform. So please keep that in mind when asking questions. Please leave patient identifiers such as name and date of birth out. And this session is being recorded for future use. It’ll be housed in this platform and hopefully, we’ll be able to make it available on pfic.org later this month.
Any questions, please put them in the chat q&a, and we will address them at the end of the session. If you run out of time, I know Dr. Thompson and Dr. Bull will be available in the panel q&a that will be shortly after this session. So I’m going to turn it over to Dr. Thompson to take it away. Thanks very much, Dr. Thompson.
Dr. Richard Thompson 02:00
Emily, thank you. So hi, everyone. I dipped into some of the talks yesterday. They sounded great, and I hope you’re enjoying and learning from the meeting so far. So as you’ve gathered, Laura Bull, my longtime colleague, is here with us on the call. But I’m going to do most of the talking on this occasion. I think she talked the last time one of these meetings was held. But we’ll both be here for questions. So I’m going to try and build on what you heard yesterday about these diseases
. I’ve it’s labeled as around genetics, but I don’t think you can separate genetics from the physiology….chemistry, what’s going on. So it’s not in isolation, so I’m afraid you’re going to get more physiology as well as genetics, to try and make sense of what’s happening and some of the things that we’re doing to try and improve these diseases. So So I do have relationships with quite a lot of companies involved in this area, which is probably a good thing, because I’m really pleased that there are so many companies interested.
And I’m going to start with this slide, which is ridiculously busy. I’ll show it again at the end and I don’t expect everyone to remember all of this, but it’s just to point out that there are lots of different mechanisms of cholestasis, from Alagille, which as you all know, is a multi system disorder associated with bile duct development problems, bile acid synthesis problems, bile acid transport problems, regulation of bile acid homeostasis, lipid transport problems, issues with the composition of membranes of cells, the maintenance of tight junctions between cells, trafficking proteins inside cells, and then actually in bile itself, the regulation of bile flow.
So we now have diseases, which involve all of those processes. So there’s no hope of me covering all of that, so in some ways, I’m going to try and simplify things. In the process, I’ll inevitably complicate things and I apologize for both in advance. So those of you who’ve heard me talk before or know anything about me know that the way I think about cholestasis does revolve around bile acids.
And they’re not the only important factor in bile formation and bile flow, but they are a key part of it. And bile and bile acids have to be put into context because, as I hope many of you know, and I hope this cartoon illustrates, and this cartoon will be sort of referred to several times in the course of my talk, bile acids undergo this enterohepatic recirculation. So within the body, bile acids are continually going from hepatocytes at the top, into bile into the intestine, across the enterocytes in the small bowel, into the portal blood and back to the liver.
And under normal circumstances, each bile acid will go around that cycle two or three times a day. Very small amounts only escape into stool and have to be replaced in the liver. And the key regulatory enzyme there is the CYP7A1 I’ve shown in the middle. And equally, very small amounts of bile acids escape this circulation, this recirculation into the peripheral blood. It’s only spillover from this and the failure of NTCP at the top left hand corner, failure of that to take the bile acids back up into a hepatocytes that causes them to appear in peripheral blood.
And as I’m sure many of you know, when we measure bile acids in peripheral blood normally, the levels are very low. And they are just what has escaped that reuptake process there. But when we measure bile acids in peripheral blood in disease, we’re not measuring them anywhere in this cycle. We’re only measuring the spillover into peripheral blood and I think that is important to remember.
Dr. Richard Thompson 06:28
So things can really essentially go wrong in two ways with respect to bile acids. We could have a problem with getting bile acids out of the liver, so there’s retention of bile acids in the liver. And of course that will, whatever is causing that, that will lead to poor bile flow and poor fat absorption and poor absorption of fat soluble vitamins.
Also, probably more importantly, the retention of bile salts in the liver will cause damage. And by mechanisms, which were discussed yesterday I know and I think could be summarized as we don’t know the answer, despite everything that Anita said, there is a relationship between retention of bile acids and pruritus, but we know it’s not a direct one. So most of the conditions we are interested in, there is a fundamentally a problem with retention of bile salts in the hepatocytes, and the failure of excretion into bile.
But there are quite a few of the diseases, which we’re going to talk about, and which none of you are very interested, where actually there isn’t a primary problem with bile acid transport at all. And so in fact, these conditions aren’t primarily cholestatic. But it’s the bile acids after they’ve been transported are causing problems in the bile ducts. So there’s these are cholangiopathies, these these are damage to the biliary tree, damage to the cholangiocytes lining the biliary tree. But bile acids are equally important there because as you know, bile is a detergent, specifically intended to help us digest fats but can harm and digest other tissues, particularly if they’re already inflamed.
So of the diseases we’re talking about, I think, obviously something like BSEP deficiency where we know the problem, and we’ll talk about it in greater detail, obviously, where there is a primary problem with bile acid transport. But I would argue that FIC 1 deficiency (PFIC type one), TJP2 deficiency, MYO5B deficiency and USP53 deficiency are really, regardless of the genetic defect, the main problem is a failure of bile salt transport out of the liver. Sometimes because there’s a primary problem with BSEP, but sometimes there is reduced BSEP function or reduced BSEP protein as a consequence of these other genes being abnormal.
Alagille is more difficult and I conveniently put Alagille in both of these categories. But of the diseases we’re going to talk about today, because there it is classified as a PFIC, is MDR3 deficiency. So it isn’t actually a form of intrahepatic cholestasis at all. There is no primary retention of bile salts or other billary constituents in hepatocytes. It’s actually a cholangiopathy. It’s damage to the biliary tree, after at least initially, completely normal bile acid transport.
The other diseases on the right there are more complex diseases, PSC, biliary atresia. They are very important to us, but they’re not forms of PFIC. And Alagille which probably is a bile duct problem. So, we will dive into these in more detail. But this graphic with the hepatocytes at the top, the enterocytes at the bottom and the bile acids going around in circles, I’m going to refer to a number of times.
Those are the major players, the major molecular components of that enterohepatic recirculation again. And in fact, from that diagram on the left, which I’ve been using so far, I will simplify it even further to the diagram on the right, which at the top shows the liver in active transport across the liver, from portal blood into bile. Bile acids then going from bile into the intestine, transported at the bottom there across the enterocytes, into portal blood and back to the liver.
What I’ve tried to demonstrate there is a normal situation, where there’s transport at both top and bottom, and free passage on the left and right, and very little escape from this circle. However, as you know, in the sort of conditions called Low Gamma GT (Low GGT) cholestasis, and I’ve already referred to these a couple of slides ago, but we’ve got the primary bile acid synthesis disorders, which are super important to us because they’re very treatable with exogenous bile acids, like cholic acid, the natural human bile acid. But they are very, very rare. And then there’s a primary problem of bile acid transport, that’s BSEP deficiency.
But as I’ve already alluded to these other secondary BSEP deficiencies where defects in other proteins, other genes are having a consequence of reduced bile acid transport. And I’m going to group all those together and call them low gamma GT cholestasis, and I’m going to call them BSEP deficiency, either primary, where the problem is in BSEP itself, or secondary, where it’s not working properly. And this is what happens in such an individual. My red circles are to try and show you there’s a restriction, there’s a failure, there’s a reduction of transport out of liver.
Consequence is the accumulation of bile salts in the liver and I’ve shown that by the large arrow at the top. And what happens in an untreated patient is that that top left arrow appears, which is spillover of bile acids into the peripheral circulation. And that’s where we measure them, as I’ve already said. So those are compartments, if there’s reduced BSEP, for whatever reason, we get bile acids measurable in peripheral blood.
Dr. Richard Thompson 12:59
So those are the pieces I want to put in place before I go into any particular diseases, as a concept in terms of bile acid physiology. But I’m now going to make life complicated by talking about a few genetic concepts. And I’m a fortunate…. unfortunately, I’m going to try and put some of the things that are still being taught in medical schools in the bin, or at least point out that they’re not as simple as people have always made out.
I think you saw something a bit similar to this in Akihiro’s talk yesterday. But mine is actually the other way around, if anything. So if we concentrate on the top figure first, my x axis, the horizontal axis, goes from no protein function on the left hand side to 100% protein and functional on the right hand side. And the vertical axis is disease free at the top and severe disease at the bottom. So a patient down here at the intersect has got no bile acid transport if it’s BSEP. But this could apply to any gene. They’ve got no residual function, and they’ve got severe disease.
Whereas a normal individual is a person at the top right hand corner, who’s got 100% function and is disease free. Now conceptually, a recessive disease really, all we know, fundamentally about a recessive disease is that if you’ve got two functioning copies, you’re at the top right hand corner, you’re fine. If you’ve got one functioning copy, you’re in the middle here, and you’re also fine. But what we don’t know about most so called recessive diseases is what happens to this curve in the left hand part here. And we don’t know whether actually, you need 45% function and the curve is somewhere over here. Or you need 10% function and the curve is over here.
And something similar is the case with so-called dominant diseases and Alagille syndrome is the only dominant disease in the ones I’ve been talking about so far. And here, the concept of a dominant disease is that if you’ve got 50% of function, where the dotted line is. If you’re a carrier, if you’ve got one mutated copy, then you should be fine. You should be disease free. If you’ve got………….. no, I’m talking rubbish aren’t I? It is the other way around. If you’ve got 50% of function, you’ve got one diseased…. you have one mutated gene, you’ve got disease. I do apologize. You need both of them to be disease free. So somewhere between 50% and 100%, is the level where you would develop disease. I do apologize for confusing you there.
However, again, we don’t know exactly where that curve is. So these curves for recessives could be anything between there and there. And dominance could be anything between there and there. But for most so called recessive diseases, for most so called dominant diseases, we don’t really know where that threshold lies, or what shape the curve is even. It turns out that, even though that’s complicated enough, not all genes, not all proteins behave in that fashion.
And there’s some that look more like this. So there’s probably severe disease where you’ve got nothing left, at the bottom left hand corner. You’re still disease free if you’re at the top right hand corner. But in between, there isn’t a threshold, but there’s a sort of continuum. So your chances of getting disease or the speed which you develop disease is related to how much protein you have, how much function you have. And here again, 50%, you’ve got a reduced likelihood or reduced speed of onset of disease compared to no protein function, but you’re not disease free.
So it’s not a single phenotype associated with a yes/no question, which is the concept of recessive and dominant conditions. Right. So that’s just how my mind thinks about the association between mutation in gene and function. And I’ll say at this point, of course, that we don’t know the relationship between these, the function and the disease, in all these diseases which we’re talking about. And although I can tell you something about this conceptually, on an individual patient basis, predicting exactly where they are on this scale is sometimes far more difficult than I’m making out now.
So this is not recessive, and it’s not dominant. Now, I think you’ve seen, we’re going to dive into bile formation in detail and look at the components of what goes wrong, and how what the disease associations are. And I think you’ve seen something similar to this yesterday. Within the liver, as you know, blood primarily flows in that direction, from the portal blood on the bottom left, to the hepatic vein, top right through the sinusoids, the blood spaces in the liver between the hepatocytes.
But then sandwiched between the hepatocytes are the canaliculi, which you’ve heard about and know about, where bile is formed, and flows in the opposite direction, into the bile ducts at the bottom left. So the canaliculus is just sandwiched space between adjacent hepatocytes. So we’ve got lots of ways of looking at that space. And this is just one of many cartoons I will use.
But it happens to show, in the middle, some of the major transporters of bile salts and bilirubin and lipids, and just shows you at the top and bottom that you actually have to seal this space and separate it from blood with these tight junction structures. The actual tight junctions are formed of claudins, which you can see are embedded in the membrane. But those are associated with proteins inside the cell. And the ones that are of interest to us particularly, are the tight junction proteins or TJPS, which aren’t intrinsic tight junction proteins but are intercellular proteins inside the cell interacting with the claudins which are part of the tight junctions.
So this is where bile is made. This is where the the components of bile first start out. And if we just look at a single membrane in that canalicular membrane, the apical membrane, the surface of the hepatocyte, these are the major players. And this is what’s happening in a normal day to day basis, is the bilirubin is being transported by MRP2, bile acids have been transported by BSEP, phospholipids are being extracted to form mixed micelles with the cooperation of MDR3. But it’s the bile acids that are really extracting the phospholipids.
But they can only do that in the presence of MDR3. Otherwise, they’ll just be digesting holes in the membrane. And at the bottom, you’ll see I’ve got FIC 1, or sorry, I’ve gone jumping too far, which we’ll come back to, which is the another lipid transporter, as I’ve already mentioned. So if BSEP isn’t working properly, and not making micelles then…….. we got there eventually…. the other transporters are there. So in particular, MRP2 is there, so that’s the reason I wanted to share this slide was because you can have very significant retention of bile salts as a consequence of BSEP deficiency, whilst still not being jaundiced because MRP2 is a separate transporter.
And it may be affected as a consequence of the retention of bile salts in the liver, but primarily, it’s not affected. So therefore, jaundice is a very, very indirect marker of disease activity, etc, in BSEP deficiency because it’s a separate transporter. And I will come back and go into much more detail shortly about the amounts of BSEP and the consequences of BSEP deficiency.
Dr. Richard Thompson 21:45
Now, I’ve already mentioned MDR3, and I wanted to talk about few minutes about MDR3, because I’ve already told you MDR3 is essential for lipid transport. And again, initially bilirubin is transported perfectly fine, and bile acids are transported perfectly fine. And that’s what I’ve been saying already. This is not a primary cholestatic disorder because those are transported.
But without MDR3, you can’t make those micelles, and what you end up with are lots of free bile acids. And these free bile acids are powerful detergents and they cause damage to the hepatocytes and the cholangiocytes lining the bile ducts. So this is a cholangiopathy causing damage to the biliary tree. But what you’ll also realize is if there’s no MDR3 working, there’s no accumulation of anything inside the hepatocytes. There’s no damage to the hepatocytes.
But what there is, is damage to the biliary tree further down. And in fact, it’s the amount of MDR3 that’s present that determines the amount of phospholipid in bile and that will determine the amount and the speed to which bile ducts are damaged. So there is no threshold. There’s no level which is going to cause an acute cut off, like for bile acids.
And this is MDR3 is really of the shape of the graph, which I showed you a few moments ago, which is one of these much more complex diseases. And so there’s patients for instance, with reduced MDR3 function, but nothing like absence, they will have reduced micelle formation, and they will have some free bile acids as a consequence. So in a patient like this, the disease will not be the severe early onset, progressive liver disease that was originally described in MDR3 deficiency, but could be a cholangiopathy presenting in several decades into life.
And in some cases, in very extreme cases, cholangiopathies are often asymptomatic until actually quite severe damage has occurred. And we’ve even seen patients who’ve got MDR3 deficiency, but have got retained functions that are exactly like this with a some micelle formation, undoubtedly and there’s enough free bile acids to cause damage to the biliary tree who are not presenting until the eighth decade, and sometimes then only with a bile duct cancer or liver cancer. Clearly, they’ve not had any symptoms prior to that.
And this makes life very complicated because MDR3 really is not behaving like the other diseases we’ve been talking about and certainly isn’t behaving in the fashion that we originally thought MDR3 was behaving, where it was a nice, straightforward, explicable disease of early childhood associated with a complete loss of function. So, as a consequence of this, you can have, if you’re at the bottom left hand corner, you can have severe early onset disease. But if you’re in the middle of somewhere, you may have very low level activity but you then become much more obvious if you’ve got some other insults to the liver, which could be hormonal in pregnancy or it could be other factors.
And the clinical presentation may be of a cholangiopathy at any age, or it may be the syndrome called LPAC, which is low phospholipid, associated cholestasis. And so in fact there, the things that cause the presentation is not the cholangiopathy, but actually the fact that with reduced phospholipid in bile, cholesterol precipitates, and forms gallstones, and not just gallstones in the gallbladder, but gallstones in the bile ducts of liver itself, which can be very difficult to manage.
That’s what LPAC is, is this intrahepatic bile duct stone formation, because of reduced phospholipids because of reduced MDR3. And from a clinical point of view, and very much from a family point of view, this is a big issue. Because, really, the children who’ve got two mutations are in the bottom left hand corner, have parents who are in the middle. And some of those parents actually do have abnormal liver function tests when the children first come and see us, but many of them don’t. They, such parents, do need follow up.
If they’ve got any abnormality of liver function tests, they need treating with ursodeoxycholic acid, particularly if they’ve got raised Gamma GT, because it’s a pretty sensitive marker of cholangiopathy in MDR3 deficiency. But this is creates quite a lot of work for everyone and a lot of anxiety for families, I’m sure. We can’t prove that ursodeoxycholic acid stops the long term problems, but it certainly improves the biochemistry in these milder cases.
And we think so far that it’s it’s it’s reducing the risk of problems later in life. But we cannot put our hand on the heart and say that is the case…. yet.
Dr. Richard Thompson 27:25
So going back to the low gamma GT diseases, the remaining one that I haven’t talked about, which we’re going to discuss today is at the bottom of there is FIC 1, PFIC type 1. And the problem here is actually this transporter is internalizing phospholipids. So those are, if you can see the membrane has gotten an inner layer on the left and an outer layer on the right. By using the different colors, I’ve shown that the composition of those two is different.
And that’s the same in all cells in the body really and unless you’ve got that asymmetry, other proteins in the membrane don’t work properly. And FIC 1 deficiency, as you know, is associated with clinical features in other organs in the body. That’s because this protein is working in those other organs. And the exact consequences it has in those organs is a direct reflection of which other proteins are not working properly, or the membrane structure is not as it should be, because of the failure of this protein moving lipids from the outer layer to the inner layer.
And so in this illustration here, I’ve shown those are the sort of brown amino phospholipids, which it transports, which are predominantly on the inner layer. But if FIC 1 is not working properly, then you start to see these lipids in the outer lab. And when that happens, it appears that the main consequence in terms of the cholestasis component, because obviously the explanation is slightly different in other tissues, but in terms of cholestasis, it reduces BSEP function.
So the BSEP is still there and if you stain for it in a liver biopsy, it is still present. But it’s not working properly because the environment in which it finds itself, in particular the lipid composition, is abnormal, because of the FIC 1 protein not working properly. his is one of the very few figures I’m going to show today of any experimental data, but it shows a laboratory experiment in which cell lines, which are actual enterocytes, so intestinal cell-like cells, and the top left hand corner is what they look like normally and they have this brushed border of microvilli on the top, which dramatically expands the surface area and allows lots of active transport across the intestine membrane.
And if you knock out or knock down in this case, the FIC 1 gene, and therefore reduce the protein dramatically, you can see that those microvilli are lost very dramatically. So the abnormal lipid composition is meaning that brush border membrane at the top is dramatically lost, dramatically reducing the surface area of the intestine, and the ability to absorb a variety of compounds. And as a consequence, you know, many of these patients do have GI symptoms as many of you know.
Dr. Richard Thompson 30:31
So going back to this diagram again, because I’m not… I don’t want to just talk about transporters. I want to talk quickly about these tight junctions. In real life, this is an electron micrograph, in real life, a canaliculus looks a bit like this. And so it’s actually full of microvilli, as well, just like that intestinal picture I showed you.
These are the microvilli in the space in the canalicular space. So all these transports I’ve been showing you so far, the BSEP, MRP2 and things like that are actually on the membrane, on the surface of these microvilli, which are sticking out from the hepatocyte surface to increase the surface area. But in this picture here, we’ve got one hepatocytes at the bottom and one hepatocyte at the top. And we’ve got these two tight junctions of left and right, the very sort of dark black structures, which are literally joining the two hepatocytes together and stopping the bile, which is surrounding these microvilli in the middle, stopping the bile leaking out down these structures at the sides, which are the spaces between the cells. So these tight junctions are essential to stop that leak.
And I’ve already told you that the actual proteins, which are probably making most of this dark color here, are claudins. So these are these very dense proteins, forming the structures joining the two cells together. Now there are patients with mutations in Claudin 1 and they have a form of sclerosing cholangitis. So the primary problem is really in the bile ducts and they have leakage of bile components and bile acids across these tight junctions into the paracellular space.
This is confusingly, tight junction protein 2 is otherwise known as zona occludens 2 or ZO-2. As I’ve already shown you, this is a cytoplasmic protein inside the cell. I’m just gonna go and close my door……………………….Sorry about that. It’s very hot in London today and I’ve got all my windows open, but one of the neighbors has been a bit noisy.
Dr. Richard Thompson 33:01
Okay, so TJP2 is this intercellular protein. It is not a claudin. And this is where it’s expressed, on the top of adjacent cholangiocytes in the bile ducts and this is the top of hepatocytes lining a canaliculus. And tight junctions are responsible for the barrier function, as I’ve already said, stopping leakage across this gap between cells. This is work done looking at different levels of claudin and the permeability of these tight junctions.
So it’s no there’s no question that if you reduce the amount of claudon, you get leakage. But the phenotype in Claudian one deficiency is actually very different from the phenotype in TJP2 deficiency. Claudin deficiency is, as I said, it’s a sclerosing cholangitis with a high gamma GT, whereas TJP2, as you know, is a form of intrahepatic cholestasis, so that’s slightly mysterious.
But it looks very much to me like what’s happening with TJP2 deficiency is actually very similar to FIC 1 deficiency, and it is absolutely vitally important, as I’ve already talked about these two membrane layers, that in FIC 1 deficiency there is transport between these to maintain the lipid composition of the canalicular membrane at the top, but also the tight junctions at the sides stop the lipids going between the basal lateral membrane and the apical membrane which are quite different in lipid composition as well.
I think it’s a failure of the compaction of the claudins, which is not having a problem with the barrier that is allowing lipids to leak across or failure to compartmentalize the apical and the top and basal lateral of the side membranes of the hepatocyte, which as I say, biochemically are quite different. So it looks like TJP2 deficiency more and more is similar to FIC 1 deficiency and is a manifestation of secondary BSEP deficiency rather than problem with leakage of tight junctions.
And the last of the low gamma GGT diseases I want to talk about at all today is MYO5B associated cholestasis. And as many of you will know, MYO5B was originally described as gene and a protein associated with intestinal failure or microvillus inclusion disease or microvillus atrophy, depending on which side of the Atlantic you live. We knew those patients had quite significant cholestasis and it took us a while, it has to said, to realize the mechanism.
And but more recently, we realized that actually there are patients with cholestasis caused by mutations in MYO5B, who don’t seem to have significant intestinal disease. And there is some suggestion that there is a genotype phenotype association. I don’t think it’s completely clear yet why some people get more of an intestinal phenotype and some people get more of a liver phenotype. But this protein is not a membrane protein at all, like most of the ones I’ve been talking about. It’s actually a motor protein. So it’s actually related to the myosins, which we have in muscle.
And it’s designed to do something similar, which is move things along actin filaments, which are sort of structural filaments within the cell. If this works, you can hopefully see in the top figure there a series of electron microscopy images, which is the head part, the top part
of the myosin molecule, walking along an actin filament. So that’s real transmission electron microscopy, which is getting to seeing what’s happening in real life. Somebody, I found this on the internet, actually has made a cartoon of one of these intracellular myosins walking along an actin molecule, which is an intracellular structural protein. And at the top, you can see it’s dragging a huge vesicle.
And there’s no doubt these vesicles, these membrane bound, called components, are how the lipids and membranes get to the surface of the cell. So it’s an essential component of assembling and maintaining the surface of the cell. And without this, there is no question and this was published a long time ago, that without this working properly, there is reduced expression of surface proteins, in particular BSEP.
So in this case, there is reduced BSEP in the surface of the cell. And it’s more because…. not because of lack of functional but actual lack of amount of BSEP. And undoubtedly, MYO5B deficiency is manifest as a consequence of reduced BSEP in the apex of the cell. So whether it is a failure of bile acid synthesis, in rare cases, but bile acid transport, in most cases, it could be primary because of BSEP deficiency, or I would argue, secondary BSEP deficiency as a consequence of these other conditions, which we’ve just been talking about.
But in all of them, you have this situation where you’ve got the retained bile salts in the liver because you’ve got a failure of transport out of the liver. You’ve got an overflow of bile salts into the peripheral circulation, as I’ve already shown you.
Dr. Richard Thompson 38:57
So we can come back to this graph. And this is what I believe is the case for BSEP deficiency…for BSEP. So if you’ve got 100% of the ideal bile acid transport, you’re on the right hand side, and you’ve got…you are disease free. Now, you could have reduced bile salt transport as a consequence of mutations in the ABCB11 gene encoding BSEP, or you could have reduced bile salt transport as a consequence of one of these other genetic defects, either reducing the expression amount of BSEP or reducing the function of BSEP.
Whichever of those it is, you need to have enough capacity to transport bile salts so that you don’t have retention of bile salts in the liver, because that’s when you start to get disease. And this figure, I believe, is realistic for the amount of BSEP that we need. So it’s somewhere around about 25% of the ideal is enough. And so long as we have that, then we’re happy. So this is the green area is where most of us exist most of the time.
And our happy enterohepatic recirculation is on the left hand side, with bile acids being transported across liver and the enterocytes, without accumulation anywhere. And so as long as you’re in the green zone, and you’ve got 25% or more of the ideal bile salt transport capacity, then you’re disease free. But obviously, if you are then in the brown zone, and this is now less than 20%, I believe, you have what we recognize as BSEP deficiency generally, or you’ve got cholestasis as a consequence of mutations in one of the other genes.
But the end result is that you’ve got less than 20% of the ideal bile salt transporting capacity, and you have persistent cholestasis. And you look like the figure on the left with high levels of bile salts in the liver and spill over into the peripheral circulation.
Dr. Richard Thompson 41:17
What you’ll notice is there’s a small gap in between, probably somewhere around 20-25% and these are patients right on the threshold. These are individuals, I should say, right on the threshold of having enough capacity. And these are people who are generally symptom free. But it only takes something else to go wrong, like the wrong drug, wrong virus, hormones, for instance, during pregnancy, and these are the people sitting on the fence and can be tipped over into cholestasis if they’re exposed to these other secondary components.
So this is what I think is everyone is either permanently at one position on this graph, or at least, they can move between different positions depending on how much function they have as a consequence of function possibly being reduced by these other drugs or other elements. Now, as you know, and I know it was discussed at length by Henkjan yesterday, we’ve been using partial external biliary diversion to treat cholestasis for a long time. So this is the classical surgical procedure where they use a loop of jejunum between the gallbladder and the anterior abdominal wall to drain bile.
And we showed first of all in BSEP deficiency, that if you can achieve that and drop your serum bile salts as a consequence of diversion, then the need for transplantation is dramatically reduced and in up to 15 years, hardly any of these patients required liver transplant. But if you fail to drop your serum bile salts, if they stay above 102, then your need for transplantation increases enormously. And so what we’re measuring though, is not….. as I’ve already told you, is actually the bile salts in the peripheral blood. It’s just the spillover that we’re measuring. It has nothing to do with actually, it’s not a direct measure of what’s happening in the liver.
And then this here, PFIC Type 1 or FIC 1 deficiency and again, if you have a surgical diversion, and drop your bile salts below 65, your requirement for liver transplantation is dramatically less. So you are happier than if you fail to get your bile salts below 65.
Dr. Richard Thompson 43:48
So what we’re doing, partial external biliary diversion, and what I believe is happening with the ASBT inhibitors, which you heard about in great length yesterday, and I’m sure has been discussed at length, is you are rescuing the situation on the left hand side, where there’s high concentrations in the liver and spillover into the peripheral circulation. You’re introducing an arrow, which is now on the bottom right, which is where you release bile acids from this cycle, either into bile in the formation and externalizing the bile in the partially external biliary diversion, or into the colon and the feces in the case of an ASBT inhibitor.
And so what you end up with is a circulation like that, which I’m calling rescue from cholestasis. And previously, in untreated individuals, you’re either in the green zone on the right hand side completely normal. You’re in the brown zone on the left hand side with permanent cholestasis or there are these people in the middle who are at risk of cholestasis. But by treating patients with partial external biliary diversion or an ASBT inhibitor, we have moved the curve. And there is now the patients in this or individuals in this blue zone, who previously were either at risk of cholestasis or had permanent cholestasis, who are now not at risk of cholestasis.
And so whether it’s partial external biliary diversion or ASBT inhibitor, you’ve gone from needing 25% of bile acid transport capacity to now you only need 5% of bile acid capacity. So that could, as long as you that curve is up at the top, and you’d reach there probably around about 5% of ideal capacity on an ASBT inhibitor or with biliary diversion, then you’re now disease free. So that’s what’s actually happened with these drugs.
And if you remember, in the first NAPPED paper of BSEP deficiency, we described the three types of BSEP and I know this was discussed yesterday, BSEP 1, 2 and 3, with 3 having no function and 1 having the most function. And unfortunately, the most difficult group is BSEP 2 because that’s the biggest group who have got some response to biliary diversion, but don’t all respond. What we’ve done is we’ve moved the curve. So these individuals haven’t been changed. We haven’t changed amount of BSEP they have. We haven’t changed their ability to transport bile acids.
What we are changed is the need for bile acids to be transported. So they’re reducing the bile acids going back to the liver and therefore the liver can cope with a lower level of transport capacity, and will at a lower level will still not accumulate bile acids in terms of the disease. This is what it looks like we’ve achieved. So I’m getting near the end. And so how do we treat patients with PFIC or different forms of cholestasis? So first of all, we can try and address the cholestasis. Try and address the issue, which is the retention of bile salts.
And I believe that’s what we’ve been doing with ASBT inhibitors and with surgical diversion. Everything else fails and we’re pretty rubbish at doing this. We can try and address the consequences of cholestasis and antifibrotics have really never got anywhere in these sort of conditions or in fact in pediatric liver disease altogether, and not much progress in adult liver disease. ASBT inhibitors are addressing the cholestasis, but do have a consequence of improving pruritus. As you know, we’ve also in the past treated pruritus fairly extensively with drugs which don’t improve the liver at all, but just address the pruritus. Whether it’s drugs antiemetics, like ondansetron, or neurologically functioning drugs like the serotonin reuptake inhibitors or the opiate antagonists like naltrexone, etc, but they are just treating pruritus.
They’re not treating the disease. But we do and still do teat the malabsorption obviously, by supplementing the bit of fats and fat soluble vitamins. What I’ve left on the bottom of that page is actually addressing the primary genetic defect, which seems like the most obvious thing to do, but of course, is the most difficult thing to do.
Dr. Richard Thompson 48:34
And I know you had Pam Vig talked a little bit about gene therapy yesterday and I’m not going to talk about it in great detail. But I am going to say that, as you know, there are now a number of different ways of doing that. And what looks like the simplest is gene editing, where you actually just go and change the patient’s own gene and put it back to what it should be. Now, that’s clearly the most elegant. It sounds perfect. Of course, in practice, we’re not quite there yet. But what is nearer it is gene replacement.
Rather than changing the patient’s own gene is actually putting in a copy, which is functioning normally. And that can be done by putting the DNA copy in and is using adeno-associated viruses, lentiviruses and also actually not using viruses at all now. There’s methods where we can deliver genes without using a virus. As many of you will know, you don’t have to deliver the actual gene. We can deliver the code, which the cell uses from the gene to make proteins, which is messenger RNA. And amazingly in the last year, many hundreds of millions of people have been treated with messenger RNA because of the many of the COVID viruses are RNA viruses and do exactly this.
They deliver the code and let the body make the protein. So we’ve proved that it’s very efficient and perfectly possible to deliver messenger RNA to make proteins in the human body. And actually, there are quite realistic possibilities of delivering protein. You can’t just give it intravenous protein, but you’ve got to put it into a suitable packaging. But there are companies working on the ways of delivering protein and some of the proteins we’re talking about BSEP, et cetera, MDR3 could well be proteins that they try and deliver in what are actually really extracellular vesicles, which are very small packets of cell membrane containing a variety of surface proteins, which can be made in a laboratory and can be given to patients.
They’re not a treatment yet, but those are possibilities as well. So actually, when it comes to replacing genes, there’s a whole variety of ways of doing that. Also and as I’m sure many of you are aware, in cystic fibrosis now, the huge interest in the last few years are a number of drugs, which are licensed, which actually don’t deliver any new genes or anything, but they deliver small molecules, which have an effect on the mutant proteins. And this is something which could well come our way. And it may be that we don’t have to, for some of these genes, boost the amount of protein very much to get a big change in the disease. So I wouldn’t discount those as a possible future treatment for some of our patients.
But just very quickly, to summarize the problems, with all those different types of treatments, they all have the gene therapy approaches have got, every single one of them has got issues at the moment still. So there is no single gene therapy approach which is perfect at the moment. So they’re either just not very efficient, or they require repeated doses, or they are just temporary, and you can’t have repeated doses, which is probably the worst. Or they risk damaging chromosomes and the genes that are already there and causing potential downstream problems.
So this is why gene therapy is not today’s cure, is because there are still still quite a lot of work to be done, because these are these limitations. And I get asked about gene therapy, obviously, a lot. And I just want to put it in context and tell you that, obviously, the liver is actually a good place to deliver gene therapy to. So that’s a good thing from our point of view.
The first diseases that are going to get treated with liver directed gene therapy are probably not liver diseases at all then. Because actually delivering gene therapy to a diseased liver is actually more complicated than a normal liver. But as you know, the liver makes lots of proteins for things like blood clotting, etc. or enzymes, which are not really essential to the liver function, but have a consequence elsewhere, whether in bleeding or consequences in the brain. And those are going to be the candidates, the initial target for most of these gene therapy techniques, because they just have proved that they can get it to work.
And it’s only once that’s been proved, proved that then we’ll move on and treat some of the diseases that we’re really interested in these actual liver diseases. So unfortunately, we’re not going to be first in the line for any of these treatments. But they have to happen as a series of events before we can move on and actually treat the diseases we’re interested in. So it’s a bit frustrating.
Dr. Richard Thompson 48:40
I’m almost there. So I showed you this exact slide at the beginning. This is just a reminder that I’ve touched on some of these. I haven’t touched on all of them. But some of these things are actual transport defects. Some of them are membrane defects. Some of them are synthesis defects. And, but many of them are manifest where there’s an abnormal distribution or abnormal function of bile acids and those are the ones we can manipulate in the moment.
And I, in my head, divide them either ones where we’ve got retention of bile salts, which is most of the diseases we’re talking about, or where there’s bile salts in bile which causing the damage for various reasons and MDR3 is the one I cite, in particular, of the conditions which really fall under PFIC. So as I said at the beginning, if I’ve made some things simpler, I’m pleased. I hope I haven’t oversimplified them. If I made other things sound more complicated, I do apologize. But I hope I have improved your understanding of some of these diseases and the way we’re now treating them and the prospects for treating them in the near future. And I and Laura will be very happy to take some questions.
Emily Ventura 55:15
Thanks, Richard. That was a really wonderful presentation. I don’t think that anybody will blame you for the complexity of the disease. I think you did a very good job explaining it to us.
Dr. Richard Thompson 55:27
Well, I can’t, we didn’t we didn’t invent them, so we can’t take the complexity of the disease, that’s for sure.
Emily Ventura 55:32
Haha. Okay, well, we’ll take that off the table then. So one of the reasons that we framed these talks this way is because when you and I first met, you know, a decade ago, PFIC was still kind of being…. PFIC was being put on the map, essentially, it seemed, and you had an idea of the spectrum of disease, the disease. And it seems like in the 10 years, you all have learned a lot in terms of the spectrum of the disease and it seems like it’s ongoing.
So I guess, you know, there’s a lot published in BSEP, and the spectrum of BSEP and what that means for treatment intervention. I guess my general question is, where do you see this going in terms of understanding the spectrum of the other subtypes, and what that means for treatment interventions in general for the other subtypes?
Dr. Richard Thompson 56:32
You’re completely right, of course. So we… things like BSEP, MDR3 to some extent and even FIC 1, obviously, we’ve seen far more of those patients. We’ve done far more work on those genes and diseases and we’ve got, we’ve learned far more about them in the last 10 years, 20 years. Some of the other ones, TJP2 et cetera, we are still at a very early stage are really getting to grips with those. We’ve got less good animal models.
We’re starting to get some in vitro models, some animal-free cellular based models, where we can start to look at those in detail. But we’ve still got quite a lot to learn about those. But at least in terms of the initial treatments, I do believe what I’m trying to get across is right is that really many of these are really consequences of BSEP function reduction, which is good, because it means we can treat them in a similar way. And in fact, you know, if you go as far as MDR3 deficiency, there’s not a problem with bile acid transport at all. But if we can reduce the concentrations of bile acids in the bile, and change the bile acids into more friendly bile acids like urso, then we actually stand a good chance of treating some of those diseases as well.
So ASBT inhibitors are definitely going to impact some of these other phenotypes. But obviously, the numbers are smaller. They are not in the initial phases of the trials. But there are patients now with MDR3, TJP2, even MYO5B in these studies, so we will get an understanding quite quickly as to whether that’s going to improve those. But logically, I think quite a number of those patients will respond to ASBT inhibitors. So that’s, even while we’re learning about the physiology in the detail, I do believe we can probably quite quickly impact on the disease in some of those other conditions as well.
Emily Ventura 58:27
Okay, so it sounds like there’s some good opportunity in treatment options, understanding the treatment options that affect specific diagnoses, you know, now going forward, which seems like a tremendous feat in itself.
Dr. Richard Thompson 58:46
It is. I mean, it’s from our point of view, and I hope everyone else’s point of view, you know, it’s literally in the last few years and it’s these studies, which are the first randomized studies in any form of PFIC. And that in itself is an achievement and the fact we’ve got positive results is clearly fantastic. So it’s not going to cure everyone and that’s why obviously, I finished saying we’re going to have to do gene therapy and all sorts of other things as well, because we’re not going to cure everyone by these. But it’s certainly a major start.
Emily Ventura 59:18
Well, thank you. I do have quite a few questions in the chat. We are over time. Are you okay if I answer the ones that are in, probably about 10 minutes, and then we can take remaining questions in the panel?
Dr. Richard Thompson 59:28
Yep
Emily Ventura 59:29
Okay. Um, so a few related to MDR3. Would you be able to point to any papers concerning the more continuous looking loss of function of MDR3 or any direction?
Dr. Richard Thompson 59:43
There’s lots of papers, and there’s some sort of reviews, but there’s, there’s they’re all in bits and pieces. There are people describing the sort of late onset adult disease, the fibrotic cholestatic hepatitis disease. There’s papers describing those papers describing the LPAC phenotype, the cholesterol gallstone phenotype. And there are papers describing intrahepatic cholestasis of pregnancy. So, you know, there’s not a perfect paper that describes all of that, but it’s the been described in many papers, really. And there’s been…there’s review articles. I can’t think of one off the top my head, but, you know, which have tried to pull all that together.
What I hadn’t mentioned today actually, we’ve now got a lot of adult patients who are being seen by my adult hepatology colleagues, because we’ve got a big interest in this, they’ve been sending them for sequencing and finding more and more adult patients with mutations in MDR3 in particular. So, you know, I think that’s, you know, this is not just theoretical. This is the real patients, and these are patients that we can now probably treat more effectively, certainly with urso. Some of them may need ASBT inhibitors, and definitely need follow up. So, actually, the number of adult patients coming out of the woodwork is going up very quickly.
Emily Ventura 1:01:07
Interesting. Okay.
Dr. Richard Thompson 1:01:09
But I can’t point to one perfect paper describing all of that, I’m afraid.
Emily Ventura 1:01:13
Okay. Well, we’ll ping you later on that. So a few more related to MDR3. So when there is sludge and gallstones could or should increasing, ursodiol dosage to help decrease or get rid of, would that help decrease or get rid of the sludge or the gallstones?
Dr. Richard Thompson 1:01:33
It does seem to help to some extent, okay. So the truth is the small amounts of cholesterol that get into bile are a problem because cholesterol is very insoluble in water and bile is mainly water. And so to keep cholesterol in solution, you have to have bile acids, and phospholipids. And the problem with MDR3 is you haven’t got enough phospholipids. Now using urso helps a little bit, but it’s not solving the real problem. And I think by diluting the bile, if you can increase bile flow, that’s reducing the concentrations of cholesterol.
So that is the only way it really helps. It’s not getting to the problem, which is the lack of phospholipid. So it’s not so much that extra bile salts are helping, because they’re not actually very good solubilizing cholesterol because they’re a less powerful detergent, urso. But it does improve bile flow and increase bile flow and so it just dilutes the bile a bit. That’s probably how urso is working.
But obviously, if the problem fundamental problem is MDR3 deficiency, then there’s a risk of damage to the biliary tree because of the bile acids on therefore, ursodiol has changed the nature of the bile acids, and so therefore, urso is probably a good idea anyway, but it’s not perfect in reducing the sludge because there’s still a shortage of phospholipid, which is necessary to keep cholesterol in solution.
Dr. Richard Thompson 1:01:35
Okay, thank you. Um, are MDR3 patients at risk for higher cholesterol? And if so, are there preferred medications recommended to reduce to reduce the higher cholesterol or should they avoided?
Dr. Richard Thompson 1:03:18
No, they’re not. As far I know, there’s no evidence that their at risk of increased cholesterol as far as MDR3 deficiency,
Emily Ventura 1:03:27
Okay, any medications to void?
Dr. Richard Thompson 1:03:31
Well, there’s lots of the lipid medications are…. have got liver side effects. So there’s none that absolutely can’t be used, but any medication which is having an effect on the liver, which certainly all statins and things like that do have major liver effects, have to be used with great caution in cholestasis. But there’s not an absolute contraindication. In fact, in MDR3 deficiency there’s one type of lipid which doesn’t appear in the in the blood as a direct consequence of MDR3 not being there. But the normal normal testing, they have normal cholesterol, generally.
Emily Ventura 1:04:04
Okay. Switching gears a little bit, what happens if the expression levels of BSEP become super physiological levels after gene therapy?
Dr. Richard Thompson 1:04:18
It’s good question. We haven’t achieved that yet. We don’t think you’ll have a problem. Because really, you need enough bile acid transport capacity to transport the bile acids that are already there. And if you if you have slightly too much capacity, the concentrations in the hepatocyte will go down.
But that shouldn’t cause increased synthesis because actually, the regulation of bile salts synthesis, although it’s happening in the liver, in healthy individuals who are not cholestatic, is regulated in the intestine. And it’s bile acids going through the enterocytes in the intestine, that are signaling back to the liver and regulating bile acid synthesis. So a slight over capacity of the BSEP may drop the concentrations in the hepatocyte, which would be great. But it’s not going to have much consequence on synthesis, so it shouldn’t cause great consequences.
Obviously, if you’ve got a 10 times too much protein, who knows what it’s going to do, because it could clog up other systems by making so much protein and impair other things. So no one’s going to want to create a massive amounts of protein. But if there’s slightly too much, if it’s not quite regulated normally, it is not going to have great consequences. To be honest, no one’s worried about that too much yet, because we need to get it working. But in general, if we ended up with slight over expression, it probably in the case of BSEP, is not going to be a big issue.
Emily Ventura 1:05:59
Okay, thanks. I have two more questions. And then we can wrap up. Another related to MDR23. In a person with only one copy of MDR3 gene, with liver enzymes being only slightly elevated, an elevated GGT, should that person be on ursodiol.
Dr. Richard Thompson 1:06:21
So obviously, if someone’s got elevated liver enzymes, they need investigating for the cause. If they’ve got one mutation in MDR3, that could be the cause but they need to exclude other important causes, and they need proper investigation. But if there’s nothing else going on, then certainly if the gamma GT is elevated then I would strongly advocate that they have ursodeoxycholic acid, probably for life. Usually, the gamma GT is the more sensitive marker, rather than the other liver enzymes.
If the other liver enzymes are elevated and gamma GT is not, then I’d be looking for definitely looking for other causes, in addition to the mutation in MDR3, because it usually points to something else. Gamma GT is usually the sensitive marker of reduced MDR3 function. And so I thought I saw something about dosage, but maybe I was dreaming.
If, if you’ve got if you’ve got probably cholestasis where you’ve got retention of bile salts, like BSEP etcetera, I would always be very cautious about using too much urso. Because if you can’t transport your normal bile acids, you can’t transport urso either. So in the conditions where there’s a bile salt transport problem, I would always caution against using too much urso. On the other hand, if the problem is in the bile ducts, and MDR3, when there’s no intrinsic problems with bile salt transport, then there doesn’t need to be such caution about the dosage of urso.
You can use higher doses of urso, more typical doses of urso in fact. Because most of the dosing of urso is based on patients with cholangiopathies with bile duct issues, to be honest. I would really be cautious about using too much urso in patients with a primary cholestatic problem, and BSEP in particular.
Emily Ventura 1:08:27
Okay. A lot to consider. One more question. How do you measure and determine the percent of protein function?
Dr. Richard Thompson 1:08:37
I did warn against that at the beginning. And I did say this is going to be the problem and if I could do that accurately in every patient, I will be so so happy. And so would, I’m sure, most of the people listening to this. It is not that simple. Those curves and working out how much you need have been arrived at by looking at the response to surgical diversion and ASBT inhibitors in lots and lots of patients and seeing which patients are susceptible to drug induced cholestasis, which patients have permanent cholestasis.
And it’s by looking at lots of different patients that I’ve come to those conclusions and be able to draw those curves. Now, what I can say is, and this is where it gets super complicated, because I didn’t touch on this at all, is in addition to the mutations, those sort of really damaging variants that we think about most of the time, some of which causes a complete loss of function, and some of those cause low levels of retained function. There are also common variants in BSEP, and in particular, there’s one called V444A. And actually, this is about 50/50 in the population. So there are equal amounts of the two versions of BSEP, so it’s really common.
But it makes a difference to the amount you have. And so there’s actually 32% of the population in North America and Europe, 32% who are homozygous for the lower amount. So they’re actually already in the middle of that graph. But they’re fine, because in the middle, you’re okay. You got to get down to about 25%. And so it’s the patients that have got one copy that’s completely damaged and the other copy has got this V444A, they’re the ones that have about 25%, because they’ve got zero on one copy, and 50%. on the other copy. The average is 25%. So that’s really where that 25% can be really nailed is because of these patients sitting right on the thresholds.
So the few patients like that, the drug induced cholestasis ones, we can say they’re right on the threshold. Then it gets more complicated, because obviously, the patients with two protein truncating mutations, the so called BSEP 3, they’re right down the bottom, so they there are as near as possible to zero. The ones where it becomes where we can again make some sort of intelligent guesses are the two common mutations, E297G, and D482G. D482G’s got slightly more, and it’s somewhere around 15-20%. And certainly, if you’ve got two copies of that, then you’re around about 20%.
And we know that some patients with two copies of D482G actually have been treated, they present with PFIC type phenotype, but have been treated with ursodeoxycholic acid only, and actually do really, really well. So they’ve got, you know, really on the right on the edge of being okay. And we know from the NAPPED studies that if you’ve got one of those two common mutations and a damaging mutation, then you’re right on the threshold.
But if you’ve got two common, other common ones, then or a common one and a missense, one, you’re in the area that responds very well to biliary diversion. So we’re only just…. there’s just a few mutations that allow us to start to work out where some people are. But unfortunately, the truth is, right now, the majority of patients have two different missense changes, and not one of those ones I just listed. And they fall into the BSEP 2 category, some of which do really well, and some of which don’t. And until we’ve got a bit more information, we’re not going to be accurately able to place within that BSEP 2 category where patients are.
That’s what everyone wants to know, because they’re the difficult ones in the middle, because some of them do really well after diversion or ASBT inhibitors and some of them don’t respond. So at the moment, and this is why I said at the beginning, I apologize, why I sort of apologized at beginning. It sounds like it’s really simple and we understand the whole thing. In principle, we understand a lot more. But on an individual patient basis, the majority of those BSEP 2 patients, we are still not possible to say exactly where they are, and whether they’re going to be a responder or not. I can only apologize for that, because we just don’t have enough data to nail that.
Emily Ventura 1:13:36
To me, I feel like a big takeaway is that genetic testing is becoming increasingly more important.
Dr. Richard Thompson 1:13:43
And we will get better… we are better, obviously. I mean, it’s only not that long ago, that we realized that the two protein truncating mutations, A) don’t respond to the diversion and now don’t respond to ASBT inhibitors almost certainly, and have the highest risk of cancer. And so clearly, that’s super priority, because those are the patients that almost certainly, at the moment, are the ones that need to go for early transplantation.
And I think clinically, that’s really important. Clearly now, we really need to focus on working out predictively, who’s going to respond well to these forms of treatments and who we need to be moving on and using other treatments, whether it’s transplantation or whether it’s more experimental treatments. And that’s the next priority. But unfortunately, we’ve still got a lot to learn, 20 years later.
Emily Ventura 1:14:39
Well, thank you for doing the learning and all of your colleagues. It’s…. we recognize that it’s come a long way. And I think knowing that you and your colleagues are continuing to learn more is hopeful to us. So we appreciate it.
Dr. Richard Thompson 1:14:56
We’ll get there.
Emily Ventura 1:14:58
All right. Well, I think that’s a good stopping point. I’ll see you in about an hour, I think or so and we’ll tackle a larger q&a. But thanks for giving us some extra time. It was a wonderful presentation.
Emily Ventura 1:15:10
My pleasure. We’ll see you later.
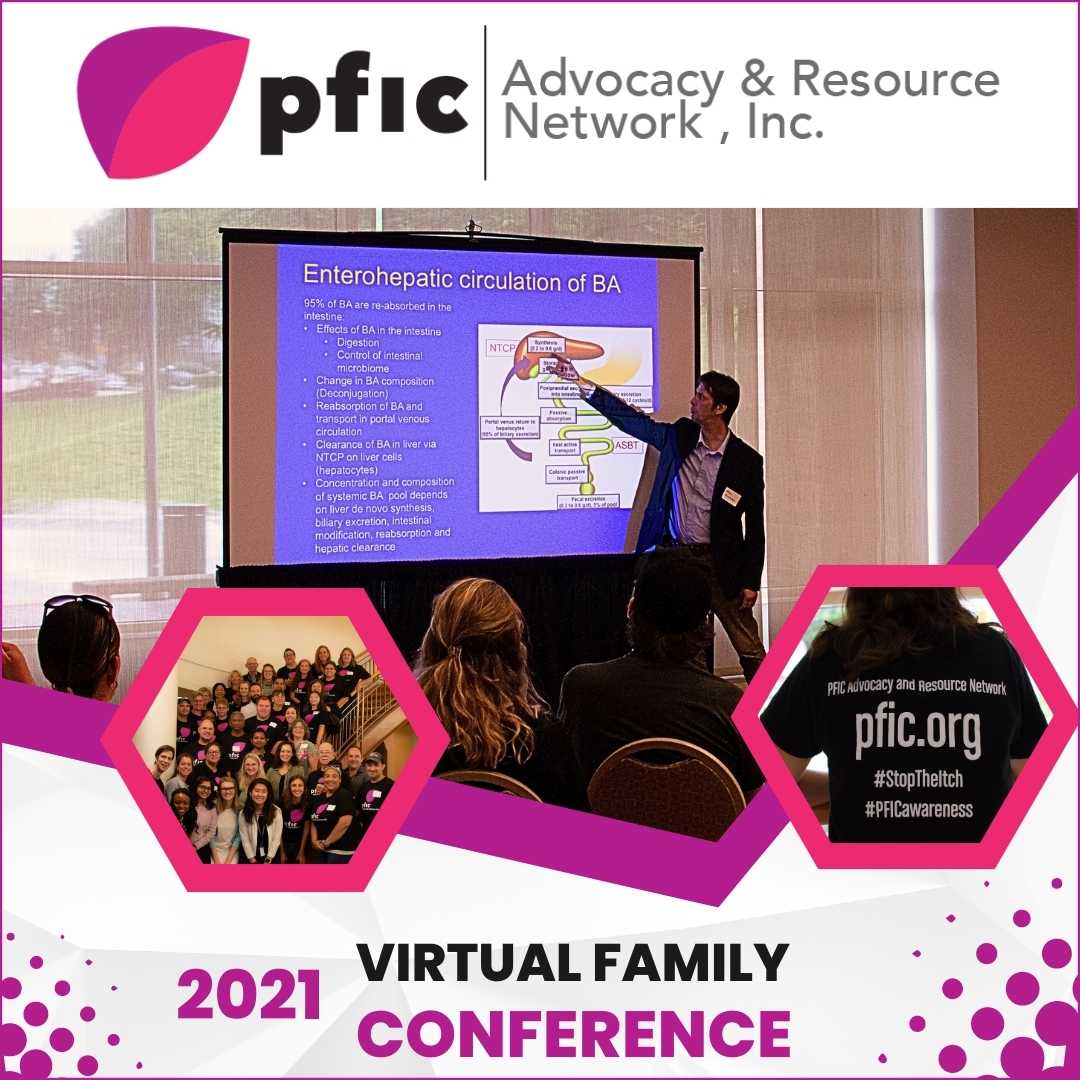
Genetics Of PFIC By Subtype
2021 Virtual Family Conference
This presentation, the second of two keynote speeches from the 2021 PFIC Network Virtual Family Conference, aims to demystify the general term of “PFIC.” It will take a deep dive into each of the genes involved with PFIC that have been identified to date, what is understood about the spectrum of each subtype of PFIC, and what still is yet to come. It is presented by Dr. Richard Thompson, a member of the PFIC Network Medical Advisory Board. Dr. Thompson is a Professor of Molecular Hepatology at the Institute for Liver Studies, Kings College London and Consultant Pediatric Hepatologist, at Kings College Hospital.
For more information about PFIC genetics and subtypes, please visit our PFIC Genetics page, PFIC Types & Subtypes page or check out this article from our PFIC Research Library.
